Glaucoma
What Is Glaucoma?
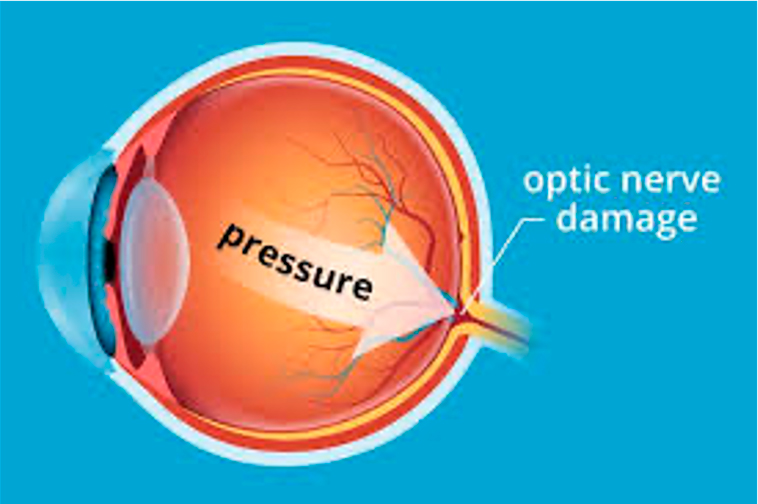
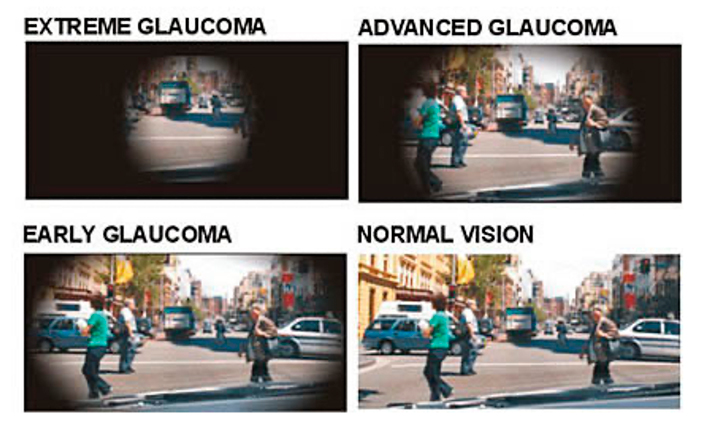
Glaucoma is a family of eye diseases that leads to progressive damage to the optic nerve. The optic nerve is a bundle of about 1 million individual nerve fibers that transmits the visual signals from the eye to the brain. People with glaucoma loose optic nerve tissue, which eventually results in vision loss. Glaucoma is scary because it usually does not cause any symptoms until it’s too late to bring back the lost vision, and it’s the second-leading cause of blindness in the United States. Glaucoma affects peripheral, or side vision, before it causes central vision loss. If left untreated, glaucoma can lead to complete loss of all vision/blindness. Although glaucoma cannot be prevented, if diagnosed and treated early, it can usually be controlled with topical eye drops.
Risk Factors for Glaucoma
- Over age 40 – though, infantile (congenital) forms of glaucoma exists
- Family history of glaucoma
- African Americans and Hispanics
- Thinner corneas
- Chronic eye inflammation
- Taking medications that increase the eye pressure such as corticosteroids (including cortisone, hydrocortisone and prednisone)
- Diabetes
- High blood pressure
- Heart disease
The American Optometric Association recommends an annual eye examination for people at risk for glaucoma. Depending on your specific condition, your doctor may recommend more frequent examinations.
Different Forms of Glaucoma
Primary Open-Angle Glaucoma (POAG) is the most common form of glaucoma. With POAG the fluid pressure inside the eye increases. This increase in pressure may cause progressive damage to the optic nerve. POAG develops slowly and without any symptoms at first. Unfortunately, many people are not aware they have the condition until they have significant vision loss.
Normal Tensive Glaucoma occurs when eye pressure remains within the “normal” range (under 21mmHg), but the optic nerve is damaged nevertheless. It is not known why this happens. People with low-tension glaucoma have an abnormally sensitive optic nerve.
Acute Angle-Closure Glaucoma (i.e. Narrow-Angle Glaucoma) is a less common type of glaucoma. It usually occurs abruptly due to a rapid increase of pressure secondary to a blockage of the drainage structure in the eye. Symptoms may include severe eye pain, nausea, redness in the eye, seeing halos or colored rings around lights and blurred vision. This is a medical emergency that can cause severe vision loss within a day of its onset. See your eye doctor immediately if you experience these symptoms.
Secondary glaucoma is a type of glaucoma resulting from an injury or other eye disease. It may be caused by a variety of medical conditions, medications, physical injuries and eye abnormalities. Infrequently, eye surgery can lead to secondary glaucoma.
Glaucoma Suspect is someone whom the eye doctor is concerned may have or may develop glaucoma because of an elevated pressure inside the eyes or an optic never with a suspect appearance.
Ocular Hypertension occurs when an intraocular pressure of greater than 21 mm Hg is measured in one or both eyes, but the optic nerves appear normal and no signs of glaucoma are evident on visual field testing. Since not everyone with high eye pressure will develop glaucoma, ocular hypertension should not be considered a disease by itself. Instead, ocular hypertension is a term that is used to describe individuals who should be observed more closely than the general population for the onset of glaucoma.
Glaucoma Diagnosis/Testing
- Tonometry to measure the pressure inside the eye.
- Pachymetry to measure corneal thickness. People with thinner corneas are at an increased risk of developing glaucoma.
- Visual Field Testing (i.e. perimetry) to check if the field of vision has been affected by glaucoma. This test measures your peripheral (side) vision and central vision by determining the dimmest amount of light that can be detected in various locations of vision.
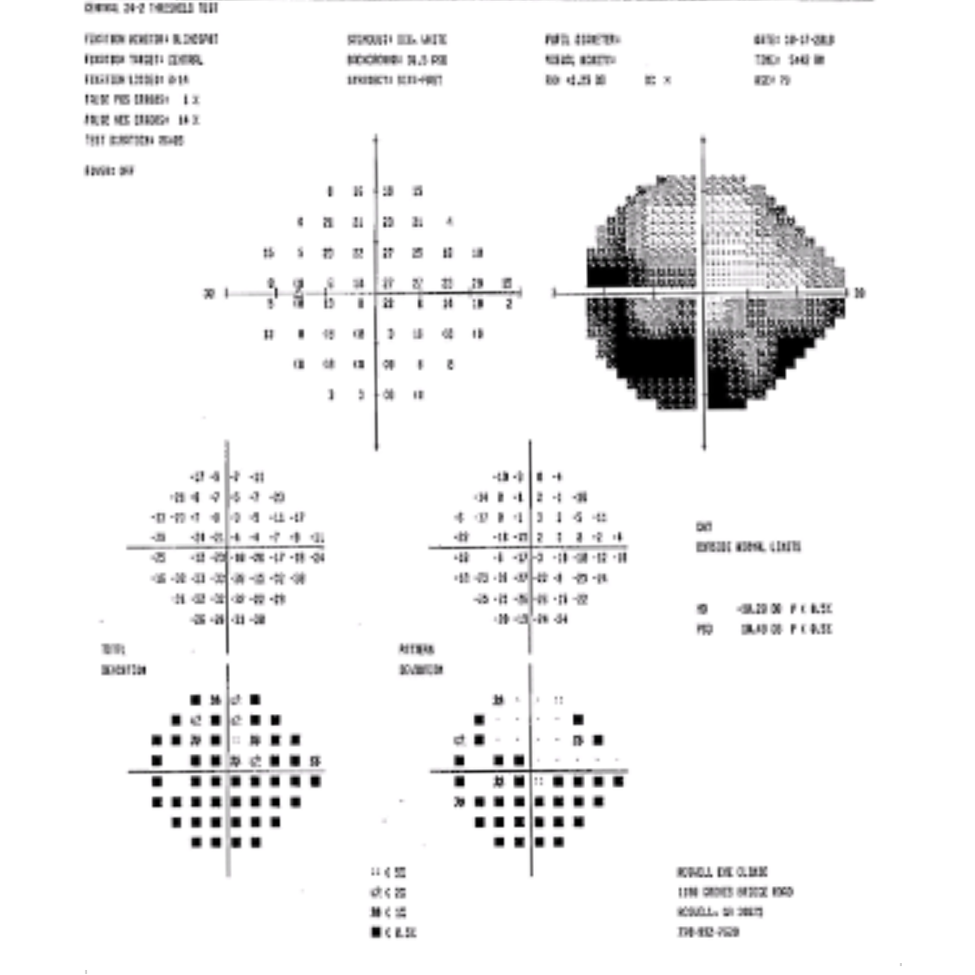
Above is a picture of a Visual Field with Glaucomatous Peripheral Field Loss
- Optical Coherence Tomography (OCT) scans is a non-invasive imaging test that uses light waves to take cross-section pictures of your retina. OCT can detect changes long before the doctor can visually see changes. Retinal Nerve Fiber Layer, the Optic Nerve and Macular for Ganglion Cell Analysis are all evaluated.
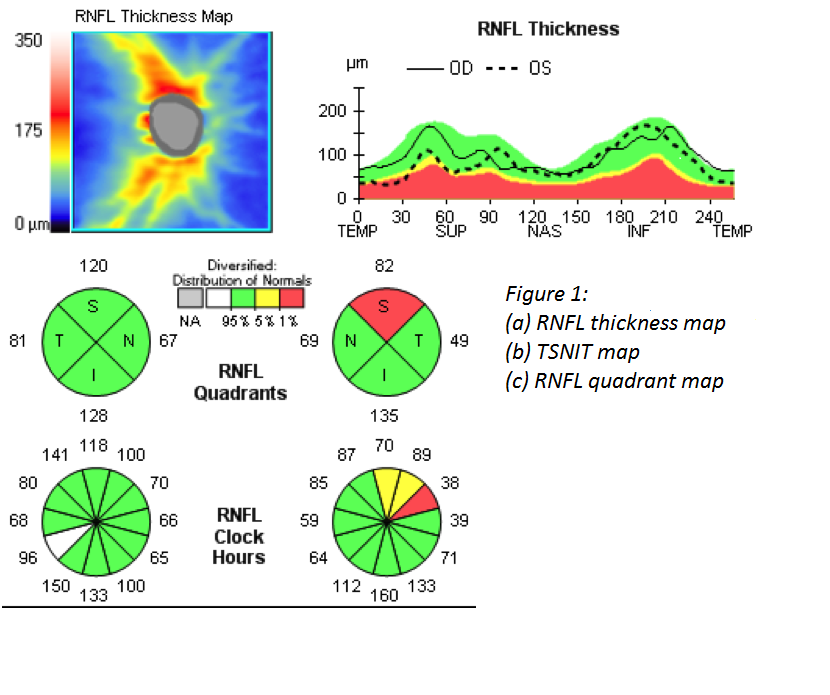
Above Is a Picture of an OCT Scan of the Retinal Nerve Fiber Layer and Optic Nerve
- Retinal Photography of the Optic Nerve to monitor any changes over time.
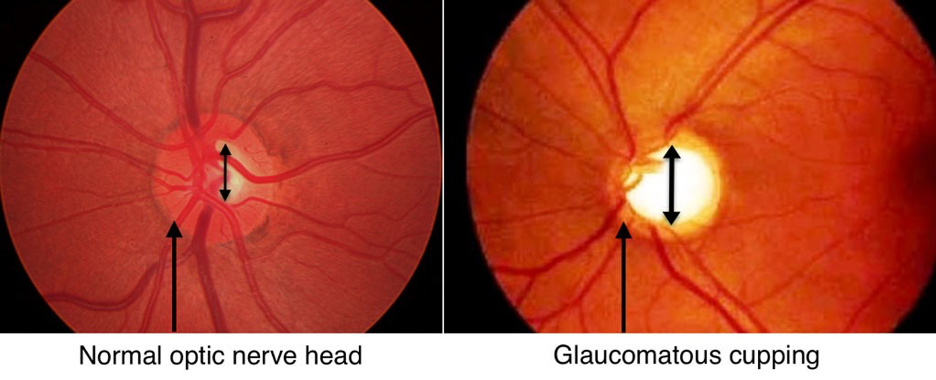
Above is a picture of a retinal photo of the optic nerve
- Gonioscopy offers a view of the angle anatomy, which is where eye fluid drainage occurs.
- Serial tonometry acquires several pressure measurements over time, looking for changes in the eye pressure throughout the day called the diurnal variation.
How Is Glaucoma Treated?
Glaucoma treatment is aimed at reducing pressure in the eye. Most commonly, use of a single prescription eye drop or a combination of several prescription eye drops are used. If prescription eye drops alone cannot lower the pressure enough, laser treatments or other surgeries may be required.
- Laser Trabeculoplasty Surgery helps fluid drain out of the eye. A high-energy laser beam stimulates the structure that drains fluid from the eye (the trabecular meshwork) so that fluid drains more efficiently. The results may be somewhat temporary, and the procedure may need to be repeated in the future.
- Conventional surgery. If eye drops and laser surgery aren’t controlling eye pressure, you may need a trabeculectomy. This filtering microsurgery creates a drainage flap. Fluid can then percolate into the flap and later drain into the vascular system.
- Drainage valve implant surgery inserts a small tube is to help drain fluid.
- Minimally Invasive Glaucoma Surgery (MIGS) work by using microscopic-sized equipment and tiny incisions. While they reduce the incidence of complications, some degree of effectiveness is also traded for the increased safety.
Acute Angle-Closure Glaucoma is treated with a laser procedure called laser peripheral iridotomy. In this procedure, a laser beam creates a small hole in the iris to allow fluid to flow more freely into the front chamber of the eye where it then can drain.
Lifelong Treatment
There is no cure for glaucoma. Patients with glaucoma need to continue treatment for the rest of their lives. Because the disease can progress or change without warning, compliance with eye medications and undergoing eye examinations are essential and treatment may need to be adjusted periodically.
Keeping eye pressure under control can slow or stop damage to the optic nerve and continued loss of vision. Your optometrist may focus on lowering the eye pressure to a level that is least likely to cause further optic nerve damage. This level is often referred to as the target pressure and is likely a range rather than a single number. Target pressure differs for each person, depending on the extent of the damage and other factors. Target pressure may change over time. New medications to help fight glaucoma are always being developed.
Early detection, prompt treatment and regular monitoring can help to control glaucoma and reduce the chances for vision loss.
Our Glaucoma Specialists: Dr. Emily Felouzis, Dr. Sarah Flanagan, Dr. Michelle Moscow, Dr. Scott Moscow, Dr. Ashleigh Sprouse