Diabetes
Diabetes
The leading cause of vision loss for Americans under the age of 74 is diabetes. Optometrists perform the majority of comprehensive, retinal eye exams for patients with diabetes in the United States and are committed to the early diagnosis and treatment to prevent blindness caused by diabetes. As of 2018, 34.2 million people (10.5%) of the U.S. population had diabetes. Of those, 7.3 million people have diabetes but had not yet been diagnosed. Often time, optometrists can diagnose diabetes in patients who did not even know they had it by examining their retina.
Diabetes is a disease that occurs when blood sugar, also called blood glucose, is too high. Blood glucose is the main source of energy and comes from food. Insulin is a hormone made by the pancreas that helps glucose get into cells to be used for energy. For patients that have Diabetes, their body doesn’t make enough (or any) insulin or doesn’t use insulin well. In turn, glucose then stays in blood and doesn’t reach their cells. Over time, having too much glucose in the blood can cause health problems. Although diabetes has no cure, steps can be taken to manage diabetes and stay healthy.
Sometimes people call diabetes “borderline” diabetes. This terms suggest that someone doesn’t really have diabetes or has a less serious case. Nevertheless, “borderline” diabetes still needs to be monitored closely.
The eye and kidney, have some of the smallest and most fragile blood vessels in the body. If someone is going to have damage from diabetes, it’s usually going to happen in the eye and/or kidney first. The eye is easier to monitor than the kidney because the eye is the only place in the body where a doctor can non-invasively visualize blood pumping in veins and arteries. In turn, all patients who have diabetes or “borderline” diabetes need to have a comprehensive eye exam at least once per year. If someone has diabetic damage to the small and fragile blood vessels in the eye, it’s a warning sign to better control his/her blood sugar before diabetic damage happens to another organ in the body such as the brain.
Diabetic Retinopathy
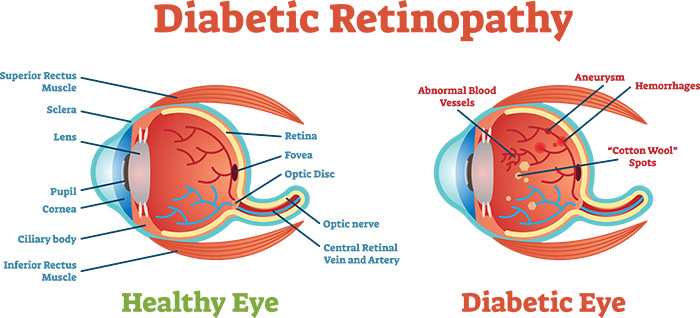
Diabetic retinopathy is a condition that may occur in people who have diabetes. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye. Diabetic retinopathy is a serious sight-threatening complication of diabetes.
Diabetic retinopathy occurs when these tiny blood vessels in the retina leak blood and other fluids. This causes the retinal tissue to swell, resulting in cloudy or blurred vision. The condition usually affects both eyes. The longer a person has diabetes, the more likely they will develop diabetic retinopathy. If left untreated, diabetic retinopathy can cause blindness.
Symptoms of diabetic retinopathy include:
- Seeing spots or floaters
- Blurred vision
- Having a dark or empty spot in the center of your vision
- Difficulty seeing well at night
When people with diabetes experience long periods of high blood sugar, fluid can accumulate in the lens inside the eye that controls focusing. This changes the curvature of the lens, leading to changes in vision. However, once blood sugar levels are controlled, usually the lens will return to its original shape and vision improves. Patients with diabetes who can better control their blood sugar levels will slow the onset and progression of diabetic retinopathy.
A comprehensive eye exam is the only way to determine if a person’s diabetes will cause blindness, which is why everyone with diabetes must have a comprehensive eye exam at least once a year. Early detection and treatment can limit the potential for significant vision loss from diabetic retinopathy.
What Causes Diabetic Retinopathy?
Diabetic retinopathy results from the damage diabetes causes to the small blood vessels located in the retina. These damaged blood vessels can cause vision loss:
- Fluid can leak into the macula, the area of the retina responsible for clear central vision. Although small, the macula is the part of the retina that allows us to see colors and fine detail. The fluid causes the macula to swell, resulting in blurred vision.
- In an attempt to improve blood circulation in the retina, new blood vessels may form on its surface. These fragile, abnormal blood vessels can leak blood into the back of the eye and block vision.
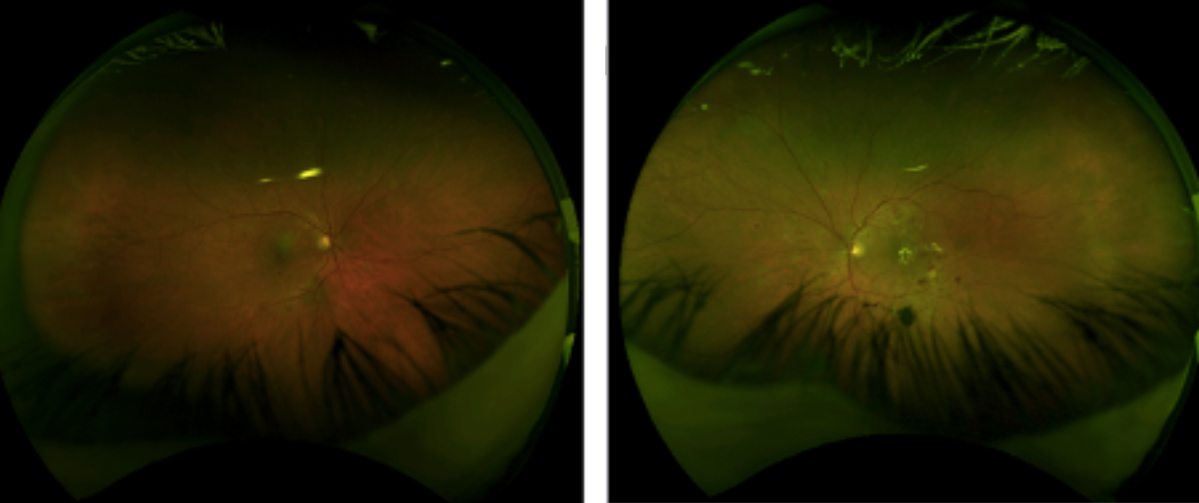
Optomap Photo of Diabetic Retinopathy
What Causes Diabetic Retinopathy?
Diabetic retinopathy is classified into two types:
- Non-proliferative diabetic retinopathy (NPDR) is the early stage of the disease in which symptoms will be mild or nonexistent. In NPDR, the blood vessels in the retina are weakened. Tiny bulges in the blood vessels, called microaneurysms, may leak fluid into the retina. This leakage may lead to swelling of the macula.
- Proliferative diabetic retinopathy (PDR) is the more advanced form of the disease. At this stage, circulation problems deprive the retina of oxygen. As a result, new, fragile blood vessels can begin to grow in the retina and into the vitreous, the gel-like fluid that fills the back of the eye. The new blood vessels may leak blood into the vitreous, clouding vision.
Other complications of PDR include detachment of the retina due to scar tissue formation and the development of glaucoma. Glaucoma is an eye disease in which there is progressive damage to the optic nerve. In PDR, new blood vessels grow into the area of the eye that drains fluid from the eye. This greatly raises the eye pressure, which damages the optic nerve. If left untreated, PDR can cause severe vision loss and even blindness.
Risk factors for diabetic retinopathy include:
- The longer a person has type 1 or type 2 diabetes, the more likely he or she is to develop diabetic retinopathy, particularly if the diabetes is poorly controlled.
- Hispanics and African Americans are at greater risk.
- People with other medical conditions, such as high blood pressure and high cholesterol, are at greater risk.
- Pregnant women face a higher risk for developing diabetes and diabetic retinopathy. If a woman develops gestational diabetes, she has a higher risk of developing diabetes as she ages.
How Is Diabetic Retinopathy Diagnosed?

Diabetic retinopathy can be diagnosed through a comprehensive eye examination. Testing, with emphasis on evaluating the retina and macula, may include:
- Patient history to determine vision difficulties, presence of diabetes, and other general health concerns that may be affecting vision
- Visual acuity measurements to determine how much central vision has been affected
- Refraction to determine if a new eyeglass prescription is needed
- Evaluation of the ocular structures, including the evaluation of the retina through a dilated pupil
- Measurement of the pressure within the eye
How Is Diabetic Retinopathy Treated?
Treatment for diabetic retinopathy depends on the stage of the disease. The goal of any treatment is to slow or stop the progression of the disease.
In the early stages of non-proliferative diabetic retinopathy, regular monitoring may be the only treatment. Following your doctor’s advice for diet and exercise and controlling blood sugar levels with oral medication and/or insulin can help control the progression of the disease.
Injections of Anti-VEGF medication in the eye are aimed at discouraging the formation of abnormal blood vessels and may help slowdown the damaging effects of diabetic retinopathy. If the disease advances, the abnormal blood vessels can leak blood and fluid into the retina, leading to macular edema.
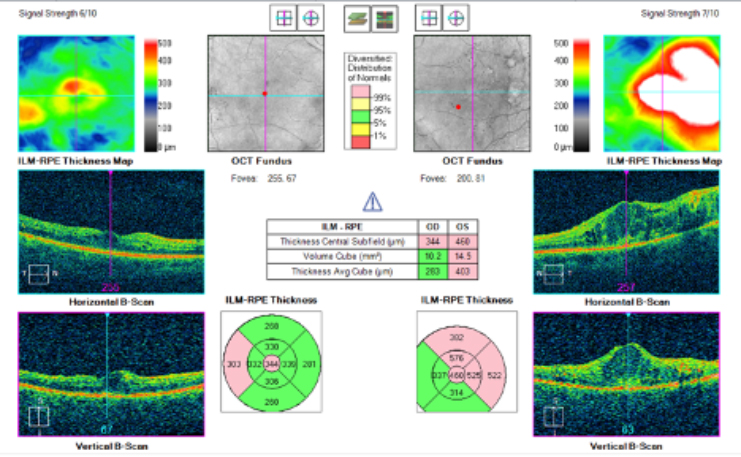
OCT Scan of Diabetic Macular Edema
Laser treatment (photocoagulation) can stop this leakage. A laser beam of light creates small burns in areas of the retina with abnormal blood vessels to try to seal the leaks. Widespread blood vessel growth in the retina, which occurs in proliferative diabetic retinopathy, can be treated by creating a pattern of scattered laser burns, called Pan-retinal Photocoagulation, across the retina. This causes abnormal blood vessels to shrink and disappear. With this procedure, some side vision may be lost in order to safeguard central vision.
Our Diabetes’ Specialists: Dr. Emily Felouzis, Dr. Sarah Flanagan, Dr. Michelle Moscow, Dr. Scott Moscow, Dr. Ashleigh Sprouse